The world changed in front of our eyes. A new virus, a new way of life, and a whole new field of medicine to navigate.
COVID-19 cracked our world wide open, and we haven’t yet managed to patch it back up. The impact it has had on every aspect of health has been overwhelming and unprecedented.
Personally, despite my work in the hospital and with dozens of patients a week, to the best of my knowledge I was able to escape infection with COVID-19 until a few weeks ago. Omnicron finally ‘got me’ (Likely my increase in socialization and waning vaccine immunity was responsible).
I spent about 3 days taking it easy, and my symptoms (while not pleasant), were comparably mild.
The most interesting to me, was the impact on my IBS. My first night of the more ‘uncomfortable symptoms’ was spent with chills, insomnia, and GI upset. I knew I had not triggered myself with any foods, therefore I suspected it was the virus.
However, in the days to follow, I continued with upper respiratory symptoms and chills, but my gut felt amazing.
I said to my husband, “Do you think COVID cured my IBS?”
Alas, probably not.
Notwithstanding my return to my ‘normal’ health in my body and my gut a week later, I wanted to know what the research and evidence has shown about IBS and COVID!
To follow is the ‘state of the science’ up to now. What we know about IBS during the time of the acute pandemic, and what we know about the post-COVID impact on GI symptoms.
The COVID Pandemic and IBS
In the time that has passed since the ‘acute’ phase of the coronavirus quarantine, we have been able to study the impact of that isolating and stressful time on the gut symptoms of our world’s population.
What we have learned is not surprising.
IBS, like many medical conditions, tends to worsen in stressful situations. Research has shown that during the pandemic, people with IBS described higher degrees of IBS symptoms. They also tended to report worse emotional and psychological well-being.
Whether those people returned to their baseline with time is not clear; therefore, see below for my tips on managing IBS symptoms.
*During the pandemic, people with IBS described higher degrees of IBS symptoms*

COVID-19 Infection, IBS, and GI Symptoms
For those infected by COVID, GI symptoms are also impacted. This is true for people with IBS and without.
First of all, having IBS (without other significant medical problems) does NOT increase your chances of acquiring COVID, and does not make you at ‘higher risk’ for COVID complications.
However, COVID does impact the gut at many levels, and therefore can worsen GI symptoms in people that contract the virus.
How does this happen? Well we have learned that the SARS-CoV-2 (the virus that causes COVID) enters the body through interaction with ACE2 receptors. These receptors are found in several parts of the body, including the intestinal tract. Supporting this, SARS-CoV-2 has been detected in intestinal cells and stool samples of affected patients.
Once the virus interacts with the intestinal lining, it may negatively affect gut function. Some potential ways include:
- Causing inflammation
- Altering the bacteria that line the intestines (also known as the microbiome)
- Changing our bodies immune responses; which can continue even after the virus appears to be gone
- Triggering emotional stress, which may increase sensitivity to gut activity
- Disrupting our intestinal ‘barrier’, impacting digestion and absorption of food
Additionally, medications and treatments for COVID, if required, may have side effects that impact our intestines (example: antibiotics).
Therefore, we recognize that IBS symptoms are likely worse during and after a COVID infection. The duration of that is unclear, read on to learn my suggestions on how to manage any GI complaints you may have.
*IBS symptoms are likely worse during and after a COVID infection*

Does Having COVID-19 Lead to Future IBS?
Whether COVID infection is linked to development of IBS is a subject that is still uncertain. We know that COVID can impact the gut, through the pathways noted above. But what happens after recovery?
One recent study looked at GI symptoms in people in the United Kingdom 6 months following COVID infection. The final sample included only 48 subjects, but almost 44% reported new onset GI symptoms, most commonly abdominal pain, diarrhea and dyspepsia.
Another group of researchers in the US looked at GI symptoms in 200 patients 6 months following COVID treatment. Seventy-nine of them (39.5%) described new GI disorders: 58 with functional dyspepsia–like disorder, two with irritable bowel syndrome–like disorder, and 19 noting both. Being female and having a history of depression or anxiety increased this risk three times, but preexisting GI issues did not impact symptoms.
As a result of the above, we speculate that there could be a ‘post-COVID IBS’ syndrome. However, it is not yet known how long it lasts, or if it develops the chronicity associated with IBS.
*We speculate that there could be a ‘post-COVID IBS’ syndrome*
Tips on Managing IBS Flares or New IBS Symptoms During and After COVID Infection
Ultimately, what matters is feeling the best you possibly can. Whether your symptoms began after COVID infection, or got worse as you navigated the new changes of life, being able to successfully treat your IBS is my goal for you.
Here are my strategies to manage IBS symptoms, during or after COVID:
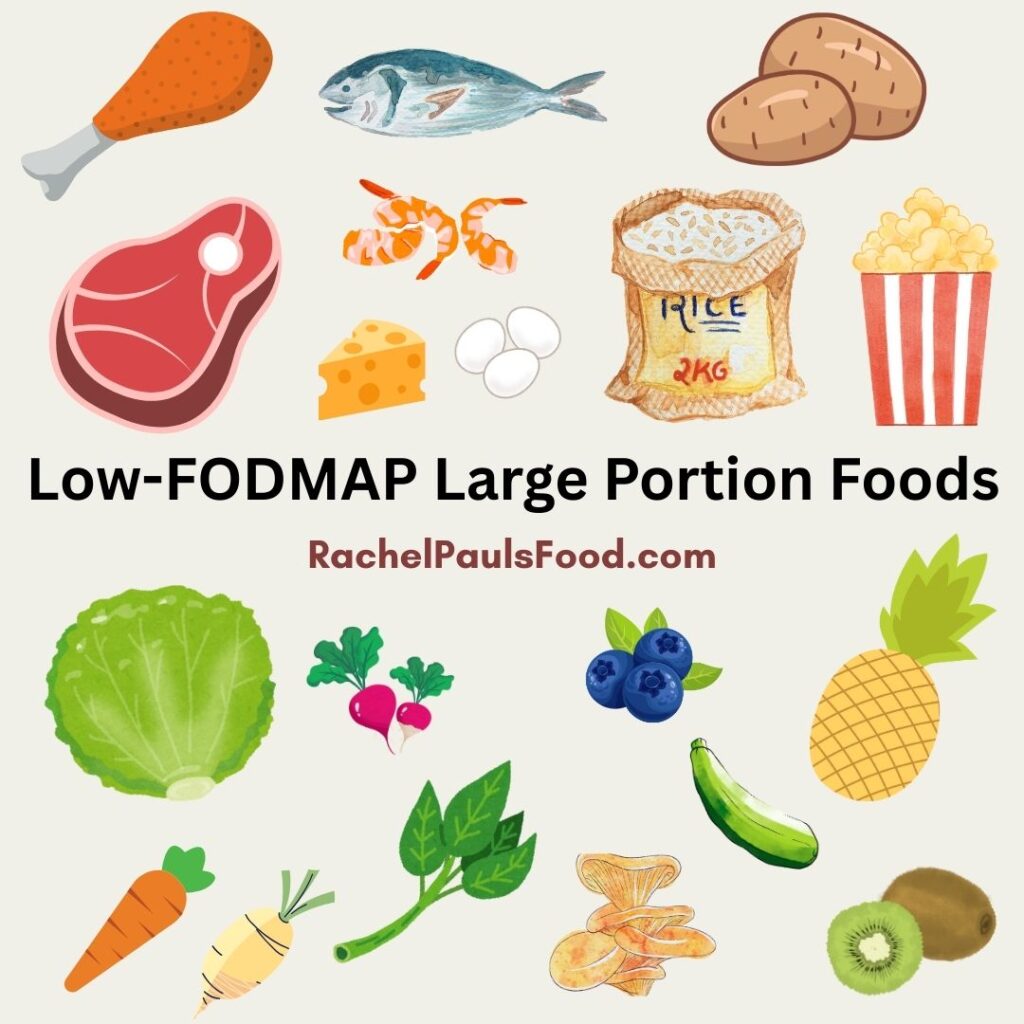
- Avoid dietary triggers: I highly suggest following a low-FODMAP diet, or a modified low-FODMAP diet, at least for a period of time until you feel more stable
- Try to reduce stressful situations. Mindfulness, meditation, and yoga have all been found to assist with IBS symptoms. Additionally, cognitive behavioral therapy (CBT) and hypnotherapy are beneficial for some patients
- Fiber may be useful for both constipation and diarrhea. Psyllium (Metamucil), methylcellulose (Citrucel), calcium polycarbophil (Fibercon), wheat dextrin (Benefiber), and acacia fiber have been noted to benefit those with IBS (constipation and diarrhea). Similarly, partially hydrolyzed guar gum (PHGG) products seem to work for IBS-D
- Incorporating probiotics has been found to reduce symptoms for some people with IBS. A great resource to peruse available options is the Clinical Guide to Probiotic Products Available in USA (www.usprobioticguide.com). Select “Adult Health” from the drop-down menu to find their probiotic recommendations for IBS
- Abdominal massage can be amazing for stimulating the intestines. This is how to do it:
- Lay on your back with your knees gently bent over a rolled towel or pillow. Place the palm of your hand on the lower right side of your belly. In a clockwise fashion, press up and around to the lower left side
- Repeat as many times as you like
- Limiting acidic foods may reduce acid reflex and dyspepsia symptoms
Most importantly, share your symptoms with your medical provider, and build a supportive network of family and friends. You don’t have to navigate your medical issues alone!
Here are some of my other favorite blogs and tips to help you with the low-FODMAP diet:
- Our 20 Most Popular Low-FODMAP and Gluten-free Easy Family Dinners
- Dr. Rachel’s Top 11 Tips & Tricks for the Low-FODMAP Diet that No One Ever Tells You
- Dr. Rachel’s Top 7 Reasons the Low-FODMAP Diet Fails and How to Fix Them
- Low-FODMAP Grocery Shopping List
- Dr. Rachel’s Low-FODMAP Diet Five Day Meal Plan, Recipes and More
- Low-FODMAP Fast Food Restaurant Options; Because Low Doesn’t Mean No
- Tips for the Low-FODMAP Vegan, Vegan Food Lists and Low-FODMAP Vegetable Stock Recipe
- Low-FODMAP Free FODMAP Guide PDF
Or peruse over 475 more low-FODMAP recipes on the blog!
Be healthy and happy,
Rachel Pauls, MD
P.S. Check out my COOKBOOK for over 100 low-FODMAP recipes, low-FODMAP Meal Plan, FODMAP Tips and everything you need!! It’s the BEST!
Be healthy and happy,
Rachel Pauls, MD

References:
-
Settanni CR, Ianiro G, Ponziani FR, Bibbò S, Segal JP, Cammarota G, Gasbarrini A. COVID-19 as a trigger of irritable bowel syndrome: A review of potential mechanisms. World J Gastroenterol. 2021 Nov 21;27(43):7433-7445. doi: 10.3748/wjg.v27.i43.7433. PMID: 34887641; PMCID: PMC8613742.
-
Gubatan J, Zikos T, Spear Bishop E, Wu J, Gottfried A, Becker L, Habtezion A, Neshatian L. Gastrointestinal symptoms and healthcare utilization have increased among patients with functional gastrointestinal and motility disorders during the COVID-19 pandemic. Neurogastroenterol Motil. 2022 Apr;34(4):e14243. doi: 10.1111/nmo.14243. Epub 2021 Aug 11. PMID: 34378840; PMCID: PMC8420203.
-
Oshima T, Siah KTH, Yoshimoto T, Miura K, Tomita T, Fukui H, Miwa H. Impacts of the COVID-19 pandemic on functional dyspepsia and irritable bowel syndrome: A population-based survey. J Gastroenterol Hepatol. 2021 Jul;36(7):1820-1827. doi: 10.1111/jgh.15346. Epub 2020 Dec 1. PMID: 33197076; PMCID: PMC7753727.
-
Cooney J, Appiahene P, Findlay R, Al-Hillawi L, Rafique K, Laband W, Shandro B, Poullis A. COVID-19 infection causing residual gastrointestinal symptoms – a single UK centre case series. Clin Med (Lond). 2022 Mar;22(2):181-183. doi: 10.7861/clinmed.2021-0522. Epub 2022 Feb 1. PMID: 35105680; PMCID: PMC8966828.
-
Quek SXZ, Loo EXL, Demutska A, Chua CE, Kew GS, Wong S, Lau HX, Low EXS, Loh TL, Lung OS, Hung ECW, Rahman MM, Ghoshal UC, Wong SH, Cheung CKY, Syam AF, Tan N, Xiao Y, Liu JS, Lu F, Chen CL, Lee YY, Maralit RM, Kim YS, Oshima T, Miwa H, Pang J, Siah KTH. Impact of the coronavirus disease 2019 pandemic on irritable bowel syndrome. J Gastroenterol Hepatol. 2021 Aug;36(8):2187-2197. doi: 10.1111/jgh.15466. Epub 2021 Mar 4. PMID: 33615534; PMCID: PMC8014795.
-
Kamp KJ, Levy RL, Munson SA, Heitkemper MM. Impact of COVID-19 on Individuals With Irritable Bowel Syndrome and Comorbid Anxiety and/or Depression. J Clin Gastroenterol. 2022 Feb 1;56(2):e149-e152. doi: 10.1097/MCG.0000000000001515. PMID: 33780216; PMCID: PMC8435039.
-
Vélez C, Paz M, Silvernale C, Stratton LW, Kuo B, Staller K; Suffolk County COVID-19 Gastrointestinal Symptom Assessment. Factors Associated With Chronic De Novo Post-Coronavirus Disease Gastrointestinal Disorders in a Metropolitan US County. Clin Gastroenterol Hepatol. 2022 Jun;20(6):e1488-e1492. doi: 10.1016/j.cgh.2021.10.020. Epub 2021 Oct 21. PMID: 34687967; PMCID: PMC8529223.