If you are a person living with IBS that also suffers from heartburn, acid reflux, and indigestion (also known as GERD/ gastroesophageal reflux disease), you are not alone.
In fact, many people have both conditions at the same time. And while these GI disorders have previously been diagnosed as two separate medical problems, newer research suggests they may be part of the same spectrum of disease. That mean, they probably have similar root causes.
Unfortunately, if you are a person with both conditions, you recognize that keeping symptoms under control is challenging. The diet plan for IBS that we know and love (low-FODMAP) does not necessarily mirror a diet suitable for GERD (low-acid). You may also notice when your IBS is flaring, it worsens your GERD.
This can be frustrating and disheartening.
Guess what? I completely understand.
I have both IBS and GERD too.
We are going to review some basics about GERD, then discuss how to manage it, including some overlapping techniques that also help IBS. These include lifestyle modifications and other therapies. Keep reading 🙂
What is GERD?
GERD, or gastoesophageal reflux disease, is a common, chronic condition that results in upper abdominal discomfort, acid reflux, heartburn, sour stomach, trouble swallowing, and/or a lump sensation in your throat. GERD may also be associated with respiratory symptoms such as coughing, or breathing issues.
GERD results when the top part of the stomach, the lower esophageal sphincter, relaxes inappropriately, or too much. This allows the acid in the stomach to leak backwards, or ‘upwards’, into the esophagus (the tube that goes from the mouth to the stomach).
Acid is a natural component of the stomach contents, and is necessary to digest food. However, acid is not meant to be in the esophagus. The acid irritation leads to pain and burning. If this acid leaks upwards into the delicate airway passages (more common at night) it will cause symptoms of asthma, post-nasal drip, and laryngitis.
Because the problem is related to acid, many treatments of GERD aim at reducing the acid in the stomach. Other therapies seek to avoid factors that encourage the lower esophageal sphincter to relax. Finally, behavior changes may cut back on the amount of acid reflux that occurs.
“GERD results when the top part of the stomach, the lower esophageal sphincter, relaxes inappropriately, or too much. This allows the acid in the stomach to leak backwards, or ‘upwards’, into the esophagus”
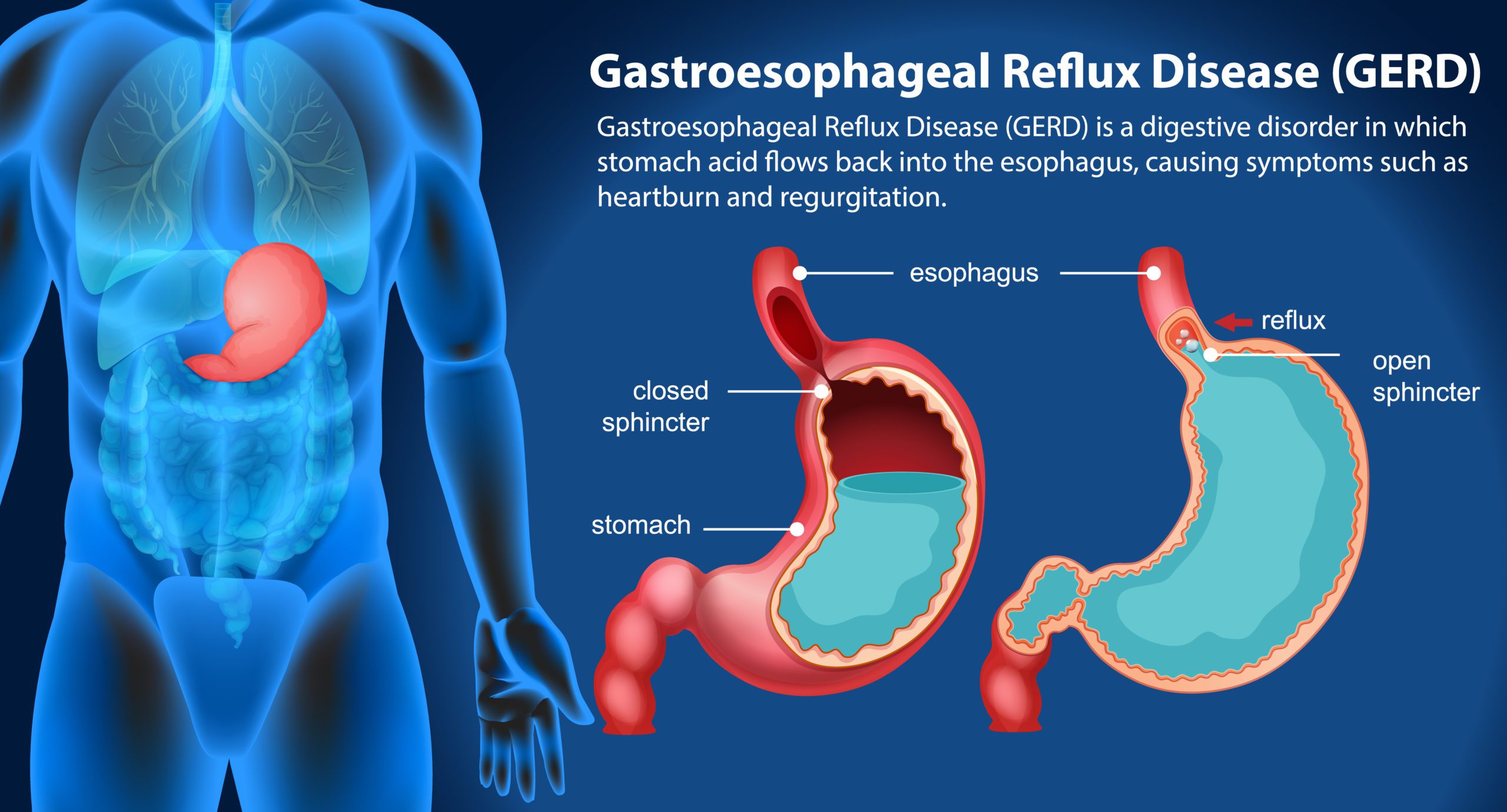 Image from FreePik
Image from FreePik
GERD and IBS
As stated earlier, GERD is a common condition in the adult population. We are also very aware of the burden of IBS, aren’t we?
In fact, approximately 40% of the world’s population suffer from a functional GI condition. Among those, 10-15% are reported to have IBS, and roughly 18-28% describe GERD.
Thus, it is not surprising that there may be some overlap. Indeed, that overlap is probably more common than just chance alone.
We now think the pathophysiology involved in causing GERD is similar to what triggers IBS. They are both disorders of motility, and thus similar risk factors are present within each group.
IBS distention also compresses, or presses on the stomach, worsening acid reflux.
Nowadays, the co-existence of IBS and GERD is well recognized. In some studies over 60% of people with IBS reported GERD symptoms; while 40% of those with GERD also had IBS.
“The pathophysiology involved in causing GERD is similar to what triggers IBS”

Treatment of GERD
If you are having some of these symptoms, I do have some positive news. We have many available ways to improve them.
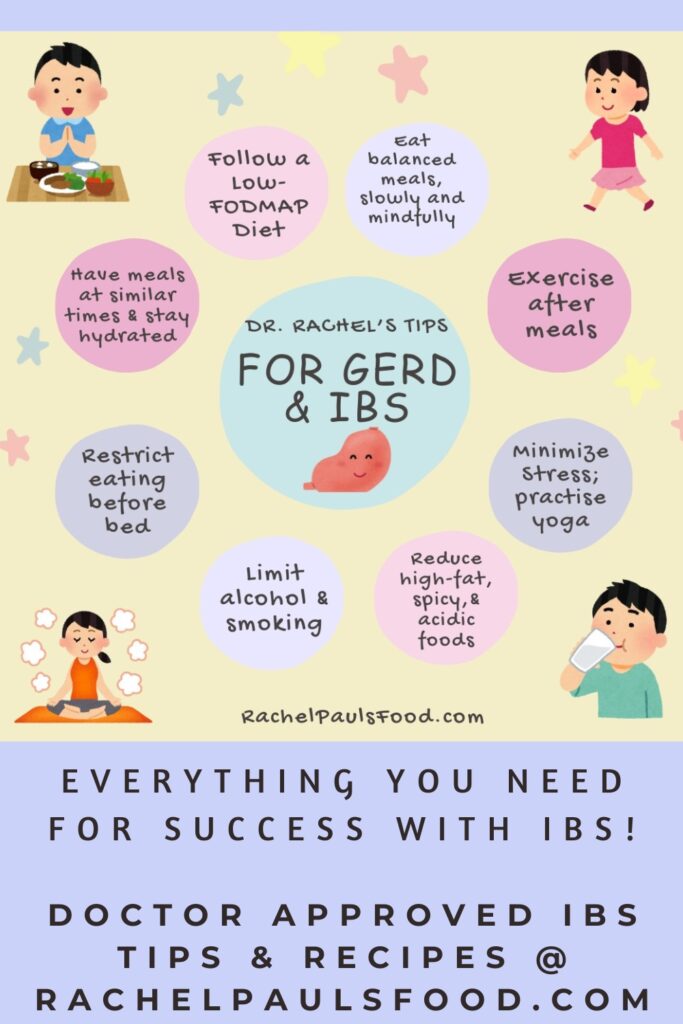
GERD treatments focus on lifestyle modifications, dietary therapy, and medications.
Lifestyle Modifications
Stress is a trigger for many medical problems. Trying to limit stressful situations, practicing mindfulness and mindful eating, as well as meditation and hypnotherapy, may help reduce symptoms of digestive discomfort.
Adequate sleep is key to keeping our bodies charged and our immune system at its best. This limits IBS flares, as well as symptoms of GERD.
Exercise is very helpful toward activating intestinal function and maintaining a healthy lifestyle. Exercise is also associated with stress reduction. Try to go for a walk daily, enjoy yoga, or sweat at a group exercise class with friends.
Cutting down, or quitting smoking is beneficial in reducing GERD. Weight loss, or maintenance of a healthy weight is also recommended. Making minor changes such as avoiding tight clothing can reduce GI discomfort. Hydrate appropriately, I recommend about 6-8 glasses of water a day.
Try to eat slowly and chew your food thoroughly. Food digestion begins from the moment we start chewing. The more the food is broken down by the enzymes in our mouths, the less work the acid in our stomach has to do. Thus, simply taking sips between bites, and chewing more thoroughly, will curb excessive acid production. Eating at predictable and consistent intervals is recommended to optimize your digestion and intestinal function.
The amount of food consumed at each meal is also important. To lessen GERD it is recommended to avoid overeating, as the distention may lead to excess acid production, and increased risk of esophageal relaxation.
Finally, is very important to modify harmful acid reflux while you sleep. Cut back on eating within 3-4 hours of your bedtime, and elevate the head of the bed to help with symptoms.
Dietary Management
There are many reported ‘trigger foods’ for GERD. However, every person is different, and just because a food is considered a triggering one, it may not be the case in your body.
I encourage you to pay attention to your personal reaction to a given food, and record symptoms as appropriate. Dietary manipulation is not as clearly beneficial for GERD as it is for IBS.
Commonly reported trigger foods for GERD and their mechanisms of action include:
- Alcohol- relax the lower esophageal sphincter
- Spicy foods- directly irritate the esophagus
- Acidic foods (citrus, tomatoes)- directly irritate the esophagus
- Caffeinated beverages- relax the lower esophageal sphincter
- Coffee- dual impact of acid and caffeine
- Carbonation- gastric distention
- Fatty food-relax the lower esophageal sphincter
- Chocolate- relax the lower esophageal sphincter
- Onion and garlic-gastric distention
- Mint and peppermint- relax the lower esophageal sphincter
You may also note these are common triggers for IBS as well. And that is a good overlap. Limiting IBS flares and reducing gas and bloating are likely to reduce GERD symptoms that can be triggered by intestinal distention. As you know- the low-FODMAP diet is perfect for that!
Working with a dietitian is of great benefit when dealing with any complex disorder of digestion. In this case, their expertise may prove invaluable. If a dietitian is not locally accessible, know that many will also provide virtual consultations.
“Working with a dietitian is of great benefit when dealing with any complex disorder of digestion”
Medications
For many people, diet and lifestyle modifications alone are not adequate to treat their GERD.
Medical consultation with a professional may lead to suggestion of over-the-counter treatments, such as probiotics, and/or supplements. It could also result in prescription of a new medication. Several medications exist to treat GERD, including those that reduce the stomach acid, improve the gut motility, or combinations of therapy.
I never suggest ‘self-diagnosis’ or excessive use of OTC treatments. If you are not improving with simple measures, then definitely get your doctor or medical provider involved 🙂
“GERD treatments focus on lifestyle modifications, dietary therapy, and medications”
Overlapping therapy for IBS and GERD
Here is a useful table that summarizes many of the therapies that commonly help both IBS and GERD:
| Intervention | Benefits for both IBS and GERD |
|---|---|
| Chew your food carefully and eat mindfully and slowly | Encourages digestion at each point in gastrointestinal tract, reduces overeating |
| Eat a varied, balanced diet | Improves immunity and overall health |
| Eat at predictable intervals | Enhances gastric emptying and digestive processes |
| Avoid over-distention of stomach, avoid large meals | Reduces discomfort and backflow of acid to esophagus |
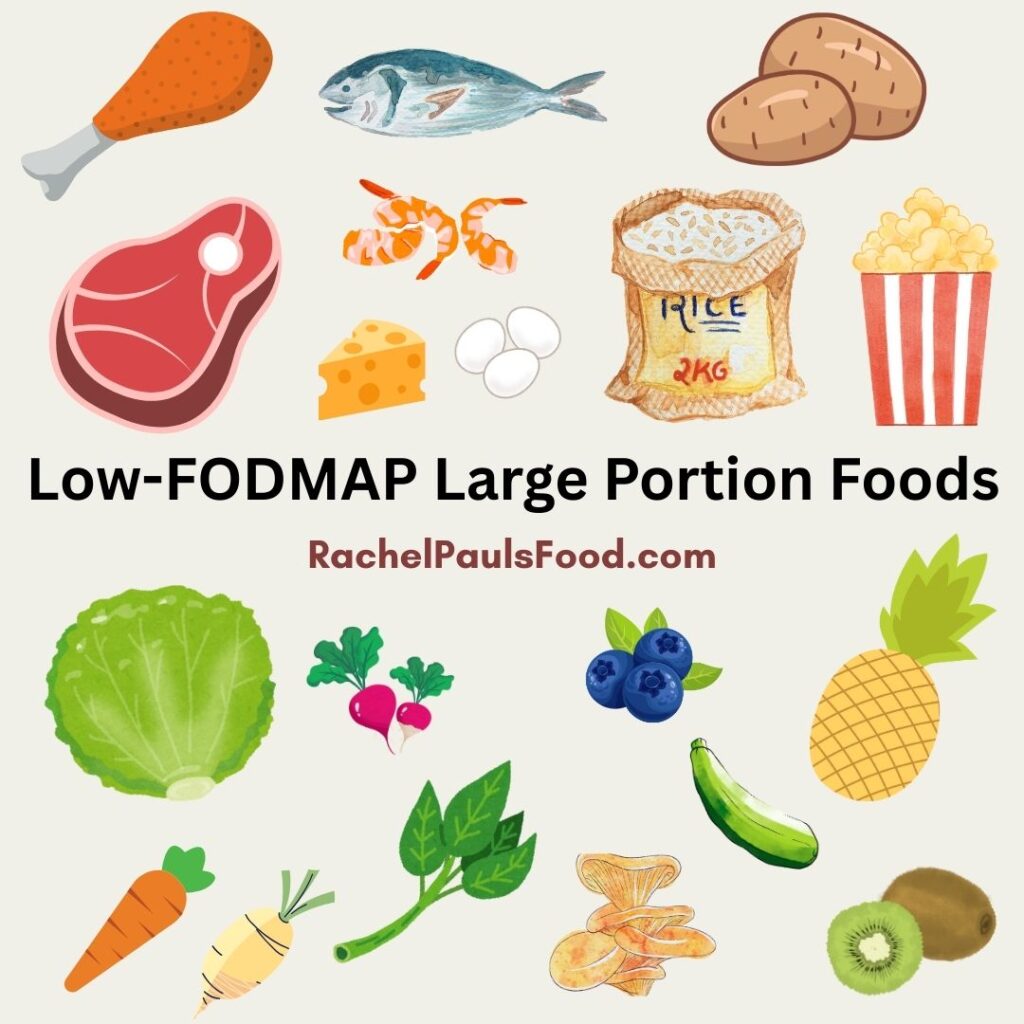
| Limit gas-producing foods (low-FODMAP diet helps with this) | Limits over-distention, reduces pressure on gut and stomach |
| Quit/Cut back on smoking | Heals lower esophageal sphincter tone, improves overall health |
| Eliminate or reduce chewing gum | Trigger foods for both IBS and GERD |
| Limit spicy and high acid foods | Trigger foods for both IBS and GERD |
| Limit high fat foods | Trigger foods for both IBS and GERD |
| Limit alcoholic beverages | Trigger foods for both IBS and GERD |
| Limit carbonated drinks | Trigger foods for both IBS and GERD |
| Reduce high fat dairy foods | Trigger foods for both IBS and GERD |
| Limit eating right before bed | Reduces gastric distention and intestinal symptoms |
| Limit stress: practice meditation; mindfulness; yoga | Boosts immunity, improves overall health |
| Exercise | Reduces stress, improves overall health |
| Stay well hydrated | Improves overall health |
| Adequate sleep | Reduces stress, boosts immunity |
As you can see, many options are available to improve both GERD and IBS! Diet is an important factor, and while the low-FODMAP diet is directed to IBS therapy, it may prove beneficial in reducing GERD symptoms too.
I have over 500 low-FODMAP recipes on my blog that can help you with selecting delicious low-FODMAP meals.
Here are some selections that are great for the combination of IBS and GERD together:
- Low-FODMAP Peanut Butter and Banana Baked Oatmeal Bars
- Low-FODMAP Chai Overnight Oats
- Low-FODMAP Salad in a Jar; Salad Bar Tips
- Low-FODMAP Cobb Salad
- Low-FODMAP Japanese Glazed Cod
- Low-FODMAP Best Steak Marinade
- Low-FODMAP Classic 3 Ingredient Roasted Chicken
You may also love:
- Low-FODMAP Best Family Meals Collection; Easy and Kid Friendly
- Low-FODMAP Best Breakfast Recipes
- Low-FODMAP Five Day Meal Plan; Recipes and More!
- Dr. Rachel’s Guide to the Low-FODMAP and Keto Diets
- Dr. Rachel’s Top 5 Tips and Food List for the Challenging Combination of IBS and IC
- Dr. Rachel’s Low-FODMAP Fast Food Options
Check out my amazing cookbooks that will guide you through all the phases of the low-FODMAP diet 🙂
Be healthy and happy,
Rachel Pauls, MD

References
Newberry, C., & Lynch, K. (2019). The role of diet in the development and management of gastroesophageal reflux disease: Why we feel the burn. Journal of Thoracic Disease, 11 (Suppl 12), S1594–S1601.
Aziz I, Palsson OS, Törnblom H, Sperber AD, Whitehead WE, Simrén M. The Prevalence and Impact of Overlapping Rome IV-Diagnosed Functional Gastrointestinal Disorders on Somatization, Quality of Life, and Healthcare Utilization: A Cross-Sectional General Population Study in Three Countries. Am J Gastroenterol. 2018;113(1):86‐ doi:10.1038/ajg.2017.421.
Sperber, A., Bangdiwala, S., Drossman, D., Ghoshal, U., Simren, M., & Tack, J. et al. (2020). Worldwide Prevalence and Burden of Functional Gastrointestinal Disorders, Results of Rome Foundation Global Study. Gastroenterology. doi: 10.1053/j.gastro.2020.04.014.
Nanayakkara, Wathsala S et al. “Efficacy of the low FODMAP diet for treating irritable bowel syndrome: the evidence to date.” Clinical and experimental gastroenterology9 131-42. 17 Jun. 2016, doi:10.2147/CEG.S86798.
Nastaskin I, Mehdikhani E, Conklin J, Park S, Pimentel M. Studying the overlap between IBS and GERD: a systematic review of the literature. Dig Dis Sci. 2006 Dec;51(12):2113-20. doi: 10.1007/s10620-006-9306-y. Epub 2006 Nov 1. PMID: 17080246.
Jung HK, Halder S, McNally M, Locke GR 3rd, Schleck CD, Zinsmeister AR, Talley NJ. Overlap of gastro-oesophageal reflux disease and irritable bowel syndrome: prevalence and risk factors in the general population. Aliment Pharmacol Ther. 2007 Aug 1;26(3):453-61. doi: 10.1111/j.1365-2036.2007.03366.x. PMID: 17635380.
de Bortoli N, Martinucci I, Bellini M, Savarino E, Savarino V, Blandizzi C, Marchi S. Overlap of functional heartburn and gastroesophageal reflux disease with irritable bowel syndrome. World J Gastroenterol. 2013 Sep 21;19(35):5787-97. doi: 10.3748/wjg.v19.i35.5787. PMID: 24124323; PMCID: PMC3793133.
Yarandi SS, Nasseri-Moghaddam S, Mostajabi P, Malekzadeh R. Overlapping gastroesophageal reflux disease and irritable bowel syndrome: increased dysfunctional symptoms. World J Gastroenterol. 2010 Mar 14;16(10):1232-8. doi: 10.3748/wjg.v16.i9.1232. PMID: 20222167; PMCID: PMC2839176.
Surdea-Blaga T, Negrutiu DE, Palage M, Dumitrascu DL. Food and Gastroesophageal Reflux Disease. Curr Med Chem. 2019;26(19):3497-3511. doi: 10.2174/0929867324666170515123807. PMID: 28521699.
Pauls RN, Max JB. Symptoms and dietary practices of irritable bowel syndrome patients compared to controls: results of a USA national survey. Minerva Gastroenterol Dietol. 2019 Mar;65(1):1-10. doi: 10.23736/S1121-421X.18.02518-7. Epub 2018 Oct 2. PMID: 30293415.








4 Responses
Thank you for this
I have been dealing with IBS-M and silent GERD for a long time. After years of eating low FODMAP and low acid, I finally got my IBS triggers identified. I thought I was doing well, and was actually enjoying eating again,vbut then went through several weeks of choking on everything I ate, so I went back to my GE for an Endoscopy with Dilation. Much to my disappointment, I learned that the lower third of my esophagus looked like a war zone. The doc has me back on a PPI, which I don’t like taking as I believe that we must have acid in our stomachs to digest properly. If I can’t digest well, I am concerned that my IBS will flare up.
To complicate matters further, in less than 2 weeks, we are leaving for 3 weeks in HA. At this point, I am very depressed about what I am going to eat. It seems from initial searches that most of what is recommended for the GERD is contraindicated by my IBS issues. I felt like I was to the point of having a lot of freedom in eating, now I feel like I have nothing I can eat.
I am very frustrated. I keep saying that I hate my own guts, but I think they hate me more. I don’t know what to do, where to get help. I have so many questions about the whole thing that people can’t answer. Like how do we know that I have lowered the acid in my stomach? What is an ideal amount of acid?
So I am very put out by the whole thing.
I am glad that I am not the only one in this state, but I sure wish there were good answers!
Thank you for sharing your story Ann. I am glad you have found a safe resource in my website.
~Rachel
I was just diagnosed with Larnygopharyngeal Reflux disease and have dealt with IBS-D for decades. I’ve been on a modified low-FODMAP diet for five years. (The only FODMAPs I can tolerate well are mannitol & sorbitol.). I’m not willing to give up my morning coffee, but I read that a small amount of baking soda in the coffee helps to reduce the PH. I assume the advice for GERD pertains to me. I love to cook, and am frusturated because I feel like there are now no safe fruits for me. Thoughts?
Hi MD Girl,
I suggest that you work with a dietitian to optimize your choices. They will be able to review your needs personally, and provide a much clearer insight. Best of luck to you,
Rachel