As a medical doctor that has been dealing with IBS for over 12 years, I have researched and practiced all the ways to manage it. Even still, I have flare ups, bad weeks, and other moments where I am not my best.
For me, a flare results in tossing and turning without sleep, trying to stop the churning and bloating. For you, it could mean locking yourself in the bathroom; or laying in bed for a week. Everyone is different.
Unfortunately, these flares rarely happen in isolation. Sure, it could be as simple as eating onion or garlic by accident at a party. But, it may also be related to subtle stresses at work, traveling, change to your sleep routine, or hormonal imbalances. So many things.
In this post, I will focus on the ways to keep your IBS in line everyday, but also during those unavoidable flares. We are going to talk about tools from a behavioral and lifestyle standpoint, and not cover OTC supplements and/or medications.
For other information, check out my post on Additive Tips and Treatments for IBS when FODMAP is not enough.
Dr. Rachel’s Behavioral Strategies to Stabilize IBS Symptoms
Dietary (Food) Modification

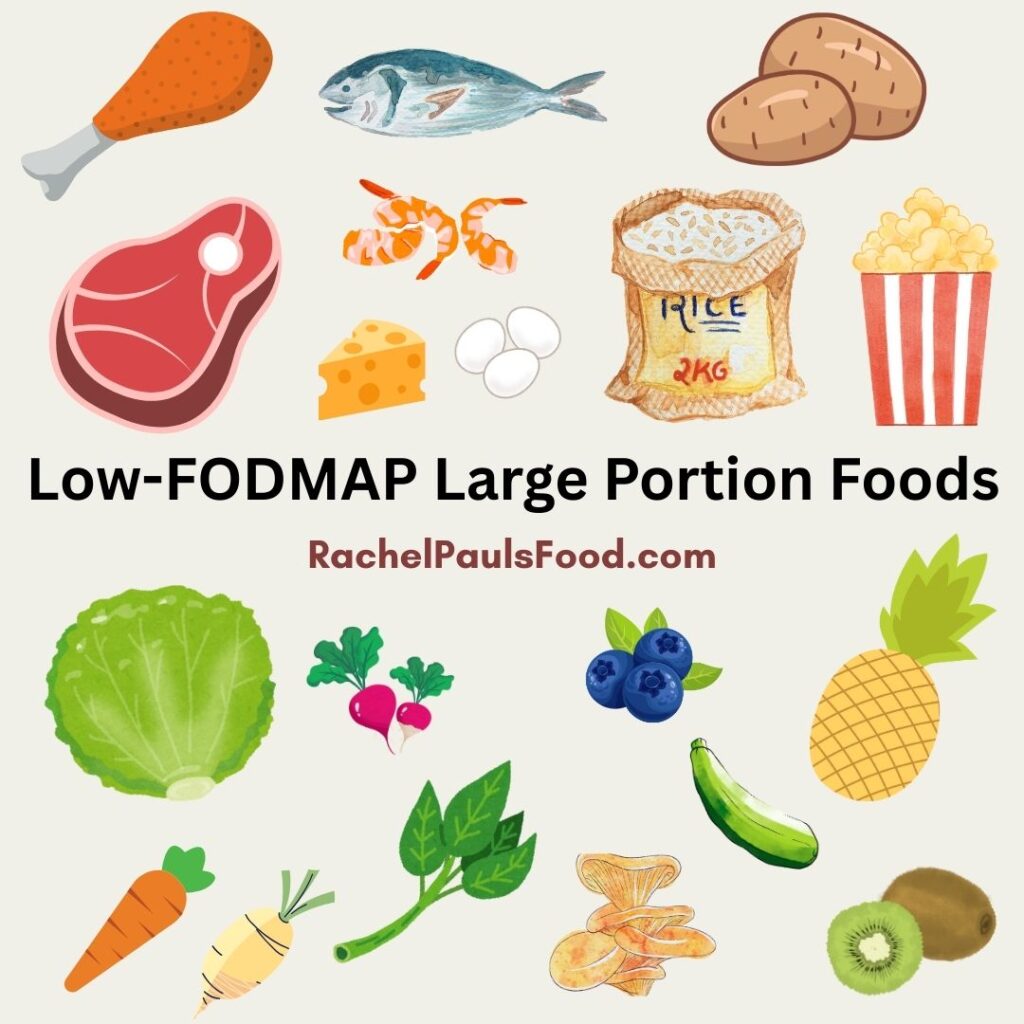
Right at the top, we need to talk about diet. Simply put, this is the most effective method to reduce IBS symptoms. Of course, you knew that, didn’t you? After all, you are at my low-FODMAP food blog already!
Studies show that people with IBS know that what they eat leads to their symptoms. The challenge is figuring out what foods those are. For many of us with IBS, low-FODMAP eating is the best way to start the healing. For others, it may be simply limiting dairy and gluten, or onion and garlic. The best way to find out, is with a (brief) elimination period, following by reintroduction.
I can walk you through the FODMAP process with my posts on Starting the Low-FODMAP Diet, and Reintroducing FODMAPs. I also have two amazing books for a detailed guide with recipes (The Low-FODMAP IBS Solution Plan & Cookbook, and The FODMAP Reintroduction Plan & Cookbook).
However, FODMAP is not the mandate for everyone. You may have other triggers that are important to pay attention to as well.
These are the common dietary triggers for IBS:
FODMAPS
One or more subgroups of the FODMAP carbohydrates is often the source for IBS symptoms, and that is essentially the basis for how the diet works. Eliminating a huge group of IBS triggers allows the body to rest and ‘reset’, so you can then reintroduce them one at a time. Eliminating high-FODMAP foods is a stepping stone for many of us to identify a personalized way of eating.
Gluten
Gluten may be linked to GI disturbances and other issues. This is independent of gluten-intolerance/celiac disease and is called ‘non-celiac gluten-sensitivity’.
Dairy
Lactose is a high-FODMAP food, but also is a trigger for gut discomfort. Other people suffer from milk intolerance or allergy, which is different from lactose-intolerance.
Carbonation
Drinks with carbonation irritate the intestines and may stimulate symptoms of IBS. This could include both soft drinks and sparkling water, to name a couple.
Spicy food
Highly spiced foods may cause both heartburn (GERD) and IBS symptoms.
Alcohol
Alcohol can lead to both diarrhea and constipation, depending on the individual. It may also lower your inhibitions around food, and increase your likelihood of eating the wrong thing.
Fiber
While many of us have been told to ‘eat more fiber’, it isn’t always the cure for our symptoms. Some fibers can be very stimulating to the intestines, while others could cause constipation. I recommend adding fiber cautiously and slowly, preferably with a medical providers’ guidance.
High fat and greasy food
Fatty foods are stimulating and can lead to increased movement in the gut, cramping and diarrhea.
Sugar and artificial sweeteners
High amounts of sugar, particularly unrefined sugars found in processed foods, can be difficult on the digestion and contribute to inflammation. Artificial sweeteners may also be hard to digest and trigger IBS.
Caffeine
Caffeine is a stimulant, and may trigger diarrhea as well as exacerbate GERD.
Acidic foods
Foods like tomatoes, citrus, vinegar, and coffee are acidic and can irritate the digestive tract. These types of foods are linked to diarrhea, cramping and acid reflux. Furthermore, many people with IBS have other conditions like GERD and Interstitial Cystitis which could flare with such foods.
Stress and Stress Management
Recent research has established several connections between our brains and our gut. Stress has an impact on intestinal motility, and can trigger flare ups of IBS, even if you are eating everything right. Although stress and anxiety don’t directly cause IBS (it isn’t in your head), they can lead to our bodies being less able to manage the symptoms and therefore trigger episodes.
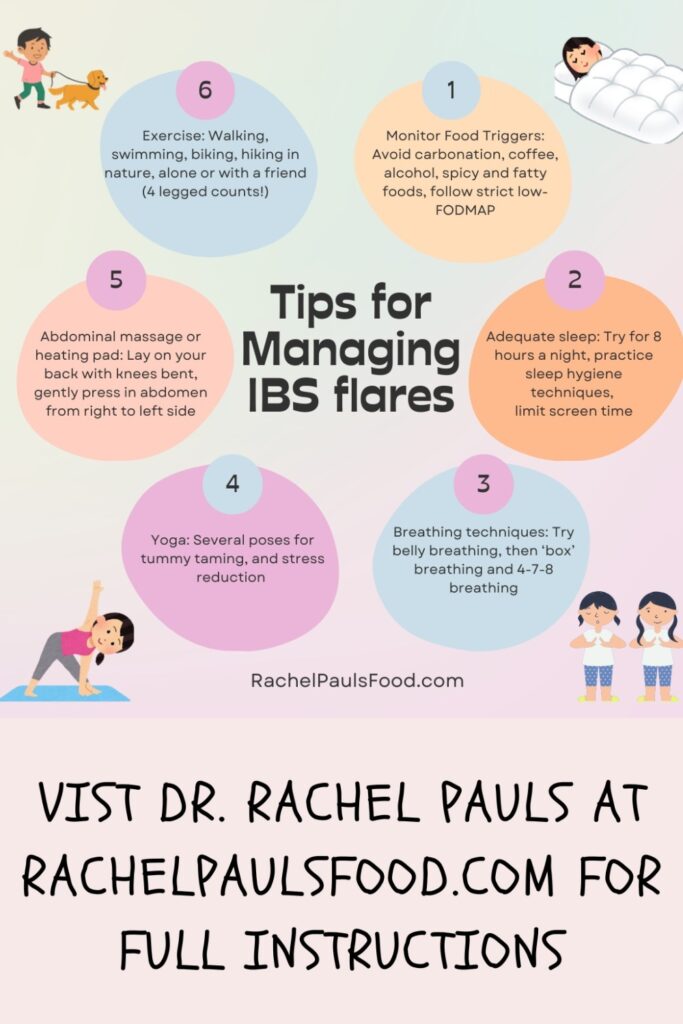
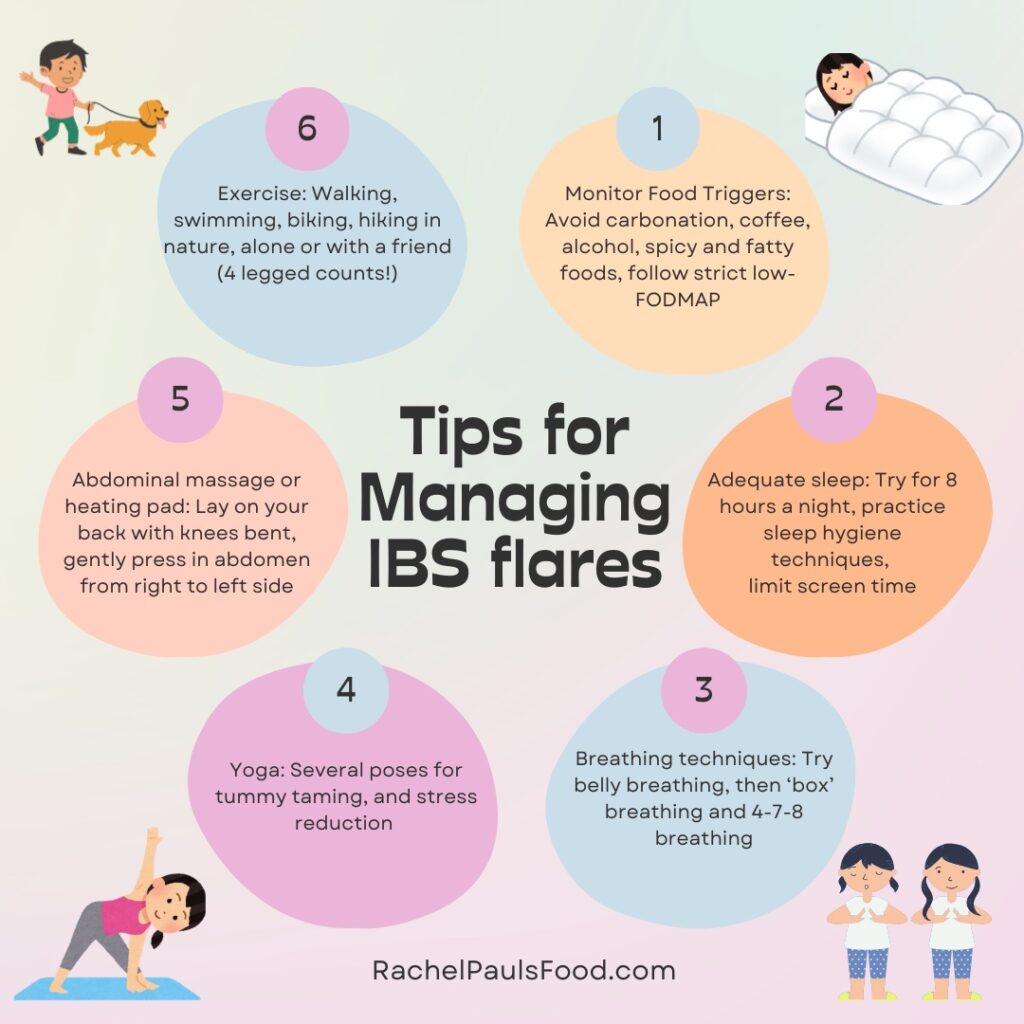
There are several ways to mitigate stress, and my below suggestions for IBS (like adequate sleep, yoga, and exercise), are clearly beneficial for it as well.
Other tools include meditation, guided imagery, and mindfulness.
I personally practice relaxing breathing techniques, to help reduce stressful moments.
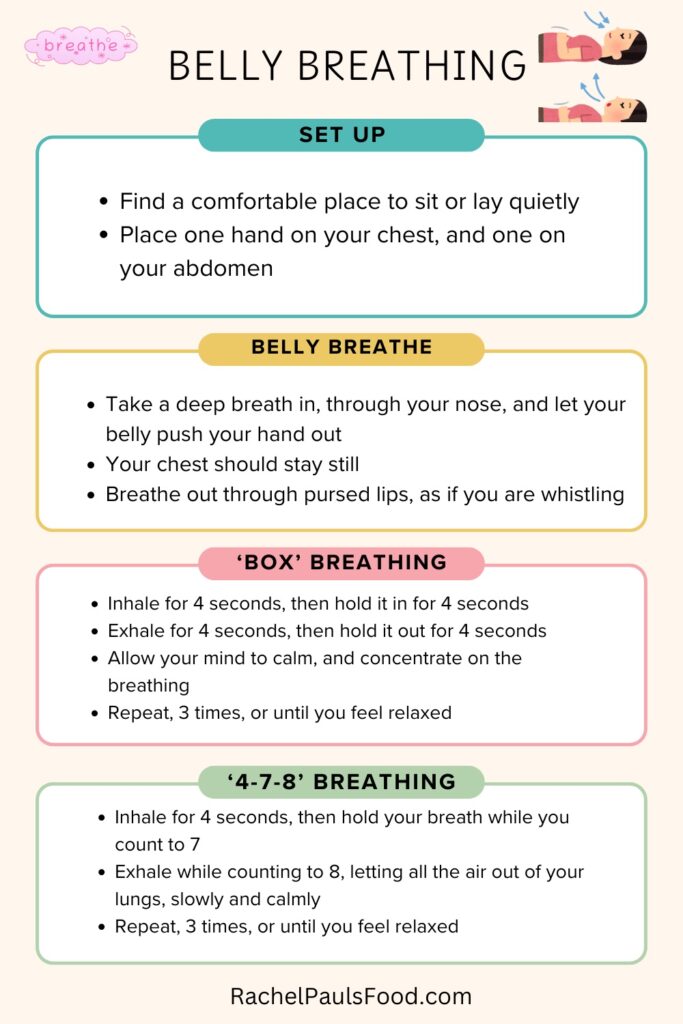
Belly breathing
A simple breathing exercise that helps release stress and IBS is belly breathing. Belly breathing expands the abdomen and soothes the gut. It also redirects the mind from any stressors.
To belly breathe, sit, or lay in a comfortable position. Put one hand on your belly just below your ribs and one hand on your chest. Take a deep breath in through your nose, and let your belly push your hand out. If you are doing it correctly your chest should stay still. Breathe out through pursed lips, as if you are whistling.
‘Box’ breathing
Next, transition to ‘box’ breathing. Time each inhale for 4 seconds, then hold in the breath for 4 seconds. You will then exhale slowly over 4 seconds, and hold your breath again for 4 seconds. Imagine you are forming a box with 4 sides. Allow your mind to calm, and concentrate on the breathing.
Do these breathing exercises 3 to 10 times, gently, and slowly.
4-7-8 breathing
Once you have mastered box breathing, advance to 4-7-8 breathing:
4-7-8 breathing involves three timed intervals of belly breathing. To start, inhale from your belly, and count to 4, as you breathe in. Then, hold your breath while you count to 7. Last, exhale while counting to 8, letting all the air out of your lungs, slowly and calmly. Repeat this exercise at least three times or until you feel relaxed. You can do it any time of day, whenever you need to feel balanced.
Exercise
Exercise is a wonderful way to improve your IBS. Try walking a bit more every day, going to the gym, joining a fitness group, or another physical activity. The movement helps propel our intestines into their natural rhythm, and encourages digestion as well as bowel movements. Plus, it will give you energy and boost your mood.
Yoga
Yoga is a discipline involving both physical and mental exercises. The physical practice strengthens and lengthens muscles, relieves joint and muscle pain, and makes your body feel good, while the mindful practice can ease stress, increase body awareness, and calm the nervous system.
There are five ‘poses’ that are of greatest help in reducing abdominal discomfort. I have a blog post that describes them. However, my favorite is ‘Wind Relieving Pose’ (Pavana Muktasana).
Pavana Muktasana
This pose improves digestion and lengthens the spine. Here’s how to do it:
- Lying on your back, bring your right knee towards your chest interlacing your fingers over your shin. Keep the other leg extended, but engaged, and your spine flat on a floor mat.
- Use your inhales to feel your belly expand into your right thigh and exhales to pull your knee in closer to your heart giving your digestive tract a gentle massage.
- Take as many breaths as you like, then transition to the opposite side and repeat.
Adequate Sleep

Getting at least 8 hours of sleep each night has been shown to decrease numerous medical issues, not just IBS. Some ways to work on your sleep hygiene include:
- Setting up a comfortable sleep environment (pillows, room temperature).
- Going to bed at the same time each day, and waking at a consistent time.
- Making sure the room is dark, without television or other screens.
- Avoiding stimulants, smoking, or alcohol before bedtime.
Mental Wellness
If managing life’s stressors seems challenging, or you are suffering from a more significant psychological or emotional disorder, then getting supportive care is fundamental to improving your IBS.
Other Behavioral Adaptations and Tips
- Smoking cessation
- Eating at regular, consistent intervals during the day
- Use a heating pad or practice abdominal massage
Abdominal massage
This is a great way to stimulate digestion and encourage gas passage or bowel movements. It works for constipation as well as bloating. Here’s how to do it:
- Lay on your back with your knees bent over a rolled towel or pillow. This posture relaxes your abdominal wall muscles and allows the massage to penetrate deeper.
- Place the palm of your hand in the lower right side of your belly. In a ‘clockwise’ fashion press up and around to the lower left side.
- Repeat this motion slowly as many times as you desire.
Gastrointestinal disorders
Treat any other contributing medical conditions (consult your doctor). Screen for small intestinal bacterial overgrowth (SIBO), gastroesophageal reflux (GERD), inflammatory bowel disease (IBD) or Celiac, and pelvic organ prolapse (POP) or pelvic floor dysfunction.
Pelvic organ prolapse and pelvic floor dysfunction
As a urogynecologist, this is the condition I commonly treat. If you have problems with stool getting stuck near the rectum or vagina, there may be a structural barrier, or blockage to the bowel movements.
Possible causes are pelvic organ prolapse (rectocele, uterine prolapse, vaginal prolapse, enterocele, or rectal prolapse), or an inability to properly relax the muscles around the rectum (pelvic floor dyssynergia). These conditions lead to the sensation of incomplete emptying, straining, a need to push around the rectum to help defecate, and rectal pressure. Symptoms could begin anytime, but often increase gradually. These disorders can occur in both women and men.
If you suspect you have one of these issues, then I recommend discussing it with your primary care provider. They may suggest a referral to a urogynecologist (like me!) or colorectal surgeon.
Beneficial treatments include pelvic floor physical therapy (YES! There are physical therapists that specialize in treating pelvic conditions), changing posture during defecation to improve stool passage (try putting your feet up on a stool in front of your commode or buy a ‘squatty potty’), and surgical options.
Keep in mind…
Remember, you are not alone. Many of us have experience similar moments/days/weeks.
Feel free to reach out in the comments below! I hope you are able to incorporate some of these ways to help improve your gut balance.
Take care of yourself, and as always,
Be healthy and happy,
Rachel Pauls, MD