I have some exciting, and interesting information to share with all of you.
Like me, you are probably keen to make your body feel better in any way you can. Well, I have some easy suggestions to improve your gut function.
I am not talking about restricting your diet. This does not involve fancy products to buy, and no new medications to take.
We are looking at simple BEHAVIORS, to encourage food digestion.
By altering some of your everyday routines, you could improve your IBS.
Sounds pretty basic, right?
Let me explain:
“By altering some of your everyday routines, you could improve your IBS”

Optimize Your Eating Style
Our intestines function in a specific manner, during and between meals. Encouraging those functions helps with our gut balance, and minimizes IBS flares.
When we eat food, our GI tract reacts with a reflex (a reflex is a preprogrammed response among the nerves of our body). The nerve reaction/reflex triggers other behaviors, and that creates a ripple effect down the road.
In this case, the reaction is called the ‘gastrocolic reflex’. It varies in intensity, but aids to propel food into and along the intestines. You can sometimes feel it.
As the food pulses into our intestines, you may have an urge to have a bowel movement (this may happen after a meal, a phenomenon that I personally find very satisfactory).
The reflex is the first positive function of eating that helps with digestion.
Dr. Rachel’s Note 1: Going for a walk, or activity after a meal can also help encourage an urge for a bowel movement
Dr. Rachel’s Note 2: A strong gastrocolic reflex (noted in certain individuals, or after certain foods) can create that feeling that food is ‘rushing through you’ and could lead to urgency and diarrhea. This is more common with triggering foods, or with certain illnesses
When we aren’t eating, or in the time period between meals, intestinal “cleansing waves” known as migrating motor complexes are triggered.
These waves help prepare the intestines for another meal and are of benefit to reducing accumulations in the gut.
This is the second good function, that happens when we are NOT eating.
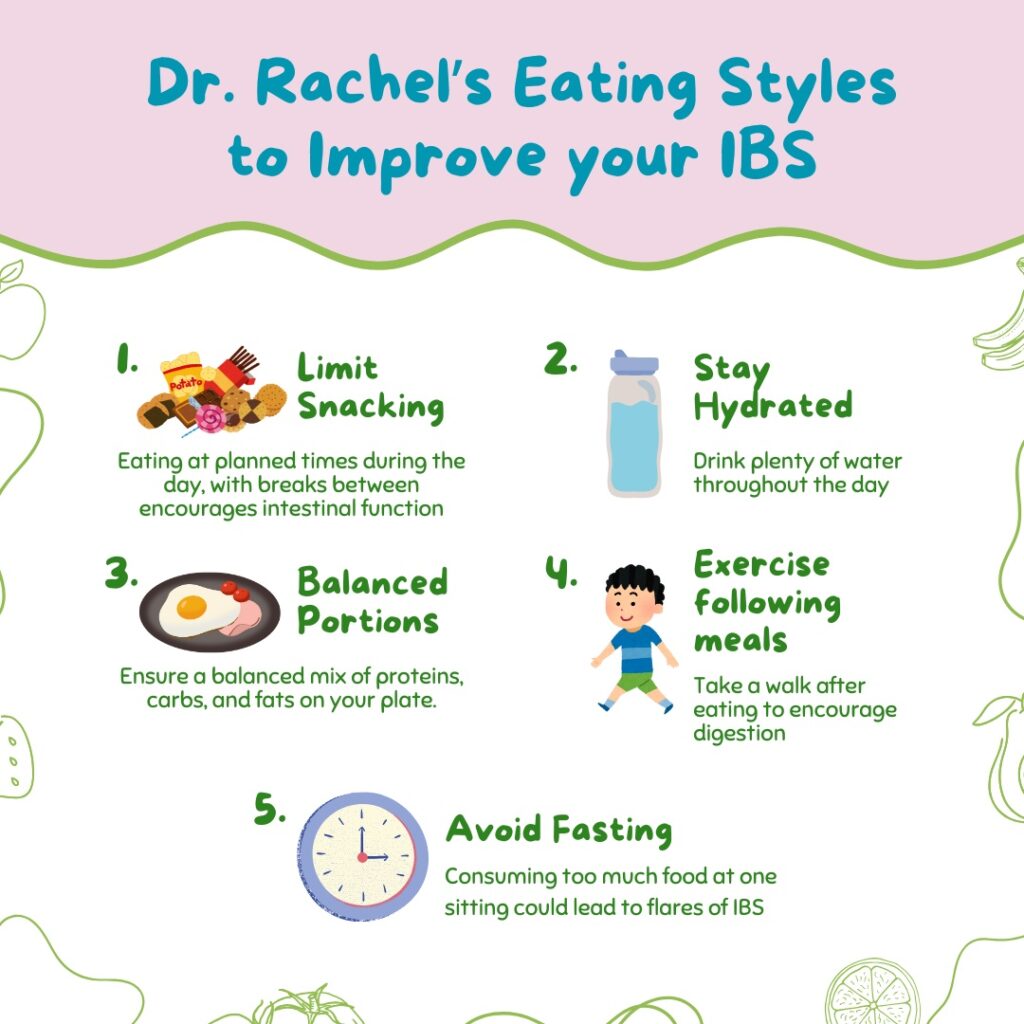
Thus, from a physiological standpoint, our intestines work best in a pattern of EATING, followed by a period of NOT EATING.
That means, it is best to take a break between meals.
How long should the break be?
I recommend about 2-3 hours after eating to optimize these intestinal waves.
That implies limiting snacks during the day.
“Our intestines work best in a pattern of EATING, followed by a period of NOT EATING”

What about Grazing?
Most people are not referring to the strict definition of ‘grazing’ when they coin this term.
Grazing means a person eats very small amounts of food in an unplanned manner throughout the day, but not necessarily when hungry.
To me, that’s the kicker. Eating when not hungry- not usually suggested, right?
Grazing eliminates the body from establishing a pattern of mealtimes and reduces the cleansing intervals.
As a result, optimal bowel functioning is impacted.
Grazing eliminates the body from establishing a pattern of mealtimes and reduces the cleansing intervals

What About Fasting?
Fasting is an eating pattern that is not new. People have been fasting for hundreds of years, across continents and cultures, for multiple reasons.
However, the behavior of ‘intermittent fasting’ has been increasing in popularity over the past few years. While there are different techniques for intermittent fasting, the practice often involves consuming a large “feast” of calories over a short period of the day, and consuming only liquids during the rest of the time. In some cases, eating is avoided for 12 hours, in other cases it could be 18 or even 24 hours.
There are multiple purported benefits of intermittent fasting. They include weight loss, reduction of diabetes, and increased longevity.
Bear in mind, I don’t recommend “dieting” while beginning the low-FODMAP diet, as there are so many other challenges to the process.
Nevertheless, when adhering to a long-term low-FODMAP lifestyle, avoiding weight loss may not be practical.
However, there is no data evaluating the efficacy of fasting in conjunction with a modified low-FODMAP diet. The only research available on patients with IBS was a small study that compared symptoms in psychiatric patients who fasted for several consecutive days with those who did not. The group that fasted had greater improvements in abdominal pain, diarrhea, and bloating, but the study had several weaknesses. I don’t think the findings can be generalized to represent results from intermittent fasting.
I also have concerns about the “feast” episode leading to a larger consumption of FODMAPs in a shorter period of time. That load of FODMAPs may not be digested well, and could result in IBS symptoms increasing.
Finally, we lack information on how fasting impacts the intestinal microbiome.
Therefore, until further research in this area has been done, I suggest avoiding intermittent fasting while treating IBS with the low-FODMAP diet.
“With the feast phase of intermittent fasting, the load of FODMAPs may not be digested well, and could result in IBS symptoms increasing”

It’s All About Balance
We have all heard this before, but balance is the key to a healthy lifestyle.
I suggest patients partake in three moderately sized meals a day and limit frequent snacking between. Avoid grazing when possible.
Eating at predictable times each day helps with gut motility and function.
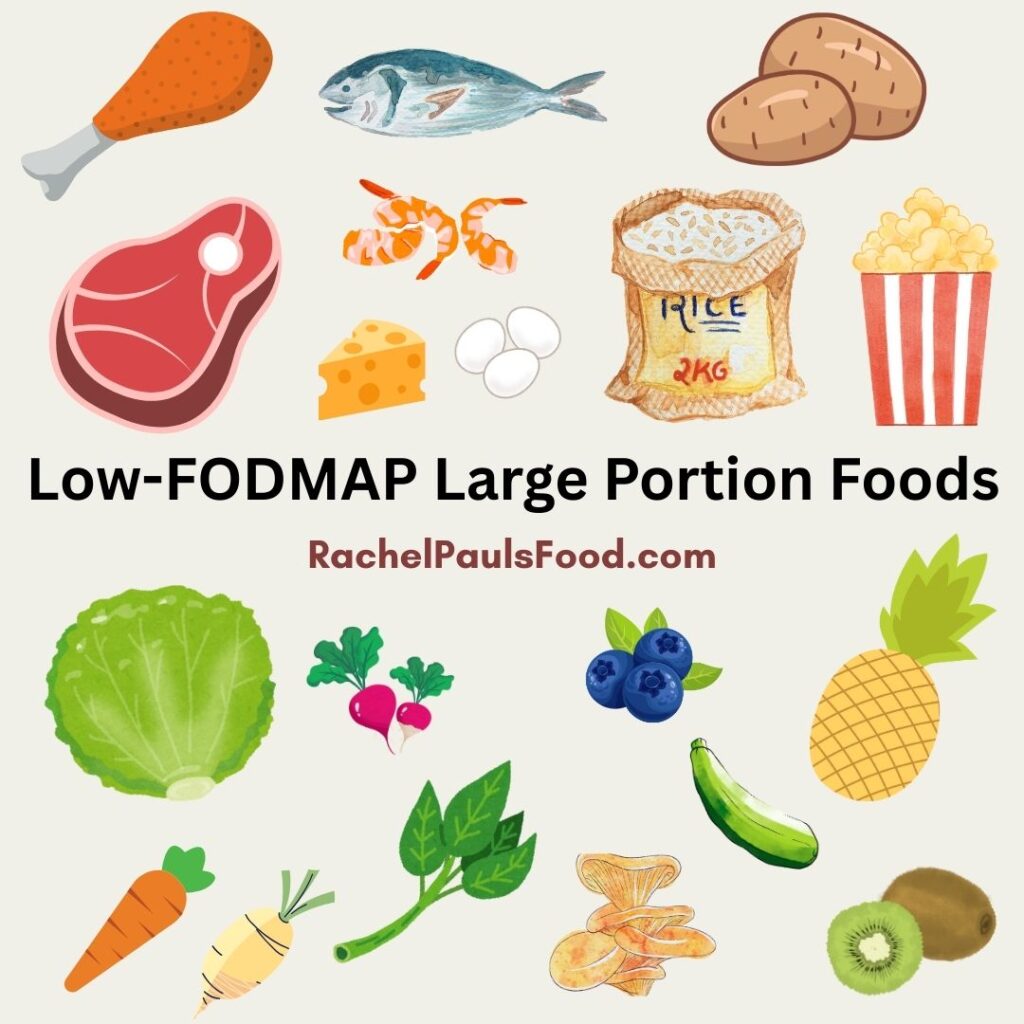
One should also strive to eat an array of fruits, vegetables, grains, and proteins each day, within the guidelines of the low-FODMAP diet.
A varied menu provides the best nutritional balance, benefits your microbiome diversity, and enhances pleasure from food.
“Partake in three moderately sized meals a day and limit frequent snacking between. Avoid grazing when possible”
The Healthy Eating Plate, as detailed by Harvard University’s School of Nutrition, describes an “ideal” meal as 50 percent vegetables and fruits, 25 percent whole grains, and 25 percent protein.
A low-FODMAP example would be:
1 cup (75 g) of steamed broccoli and carrots
1/2 cup (80 g) of baked potato, quinoa, or brown rice
1/4 cup (60 g) of fish, chicken, or beef, cooked in olive or avocado oil
Other habits to improve digestion include eating slowly and mindfully. Take smaller bites, and sip water or converse between each one. Share meals with others, to improve the experience overall.
“Mindful eating” implies living in the moment of the experience. When you are mindful you focus on your body-related sensations with heightened awareness. The goal is to promote a more enjoyable meal experience. That means turning off your phone, television or screen and savoring the mouthfuls!
Remember, our bodies are not individual organs acting alone, but a system as a whole, functioning in unison. Having good gut function will also result in greater mood, and vice versa. Be kind and patient with yourself as you learn about what makes you feel better, and understand that this is a process.
For other great low-FODMAP tips and diet inspiration, you may want to read:
- Dr. Rachel Talks the Low-FODMAP and Mediterranean Diet; Eating for Health and a Happy Gut
- Dr. Rachel’s Top 11 Tips & Tricks for the Low-FODMAP Diet that No One Ever Tells You
- Dr. Rachel’s Top 7 Reasons the Low-FODMAP Diet Fails and How to Fix Them
- Low-FODMAP Grocery Shopping List
- Dr. Rachel’s Low-FODMAP Diet Five Day Meal Plan, Recipes and More
- Low-FODMAP Fast Food Restaurant Options; Because Low Doesn’t Mean No
- Tips for the Low-FODMAP Vegan, Vegan Food Lists and Low-FODMAP Vegetable Stock Recipe
- Low-FODMAP Free FODMAP Guide PDF
- Dr. Rachel’s Guide to the Low-FODMAP and Keto Diets; 5-Day Meal Plan, Recipes & More
For other amazing ideas, see over 500 FREE low-FODMAP recipes on the blog. IBS and gut friendly!
Be healthy and happy,
Rachel Pauls, MD