As a woman officially categorized in her late 40’s (my daughter gleefully reminded me on my last birthday), I am beginning to wonder what the future years mean for my IBS control.
Is my IBS going to worsen?
Is this already happening?
I am well aware of the impact that my monthly cycle can have on my symptoms (also see my blog on IBS and PMS); but menopause sounds even scarier to me.
I decided the time had come to revisit the data!!
Given the fact I am a specialized gynecologist (urogynecologist), you would think I would know all of this already…but when it comes to my own body, I like to hear it again 🙂
What is menopause?
- Menopause is the cessation (stopping) of the woman’s menstrual cycle. It is officially diagnosed once you have gone 12 months WITHOUT a period, however, if you have had a hysterectomy, ablation, or use an IUD (intrauterine contraceptive device, like Mirena) that may be tricky to know. In those cases, your symptoms may make you aware that you are going through this change. Occasionally, blood tests ordered by your doctor may shed light on your personal hormone levels.
- The loss of menstrual cycles happens because your ovaries are not consistently ovulating (releasing an egg). This may be sporadic for a while, prior to stopping altogether. When the ovaries stop ovulating, your body will stop producing the majority of your estrogen and progesterone. Testosterone levels will also begin to drop more steeply.
- For most women, this transition occurs in their early 50’s, while others may begin having symptoms much earlier.
- Regardless of the timing, these fluctuations in hormones can lead to many changes inside of your body.
“We know that IBS symptoms increase and decrease (or ‘fluctuate’), depending on female hormone levels”
What symptoms occur with menopause?
- Some women have NO symptoms, while others have many. These range from hot flashes and night sweats, to significant depression, fatigue and weight changes.
What happens to IBS during menopause?
- Many studies have suggested that IBS symptoms increase and decrease (or ‘fluctuate’), depending on female hormone levels. This is because estrogen and progesterone impact the motility in the intestine, as well as its sensation. These hormones also play a role in inflammation. Thus, a sudden drop in hormones could result in worsening symptoms.
- A further factor that could contribute during menopause is the many overall changes going on in your body. Symptoms such as night sweats could result in less sleep, higher stress levels and increased susceptibility to an IBS flare.
- That being said, there are NOT a lot of published studies that have focused on menopause and IBS. The available data is not conclusive, with some research suggesting patients get better with menopause, and others reporting that symptoms worsen. It is also unclear whether those worsening symptoms are for a short-term period only.
“There are NOT a lot of published studies focusing on menopause and IBS. The available data is not clear-cut: some research suggests patients get better with menopause, and others report that symptoms worsen.”
What can you do if your symptoms worsen with menopause?
- Unfortunately, there is no ‘cure’ for menopause. It is inevitable. Sigh. However, hormone replacement may be useful for symptom control, depending on your personal and medical health (discuss this with your doctor). That being said, hormone replacement has not been found to directly improve symptoms of IBS, and should be initiated only under a doctor’s direction.
- My suggestion is to consult with your doctor to improve as many of the symptoms that you are able, as well as work to limit triggers for your IBS. See below!
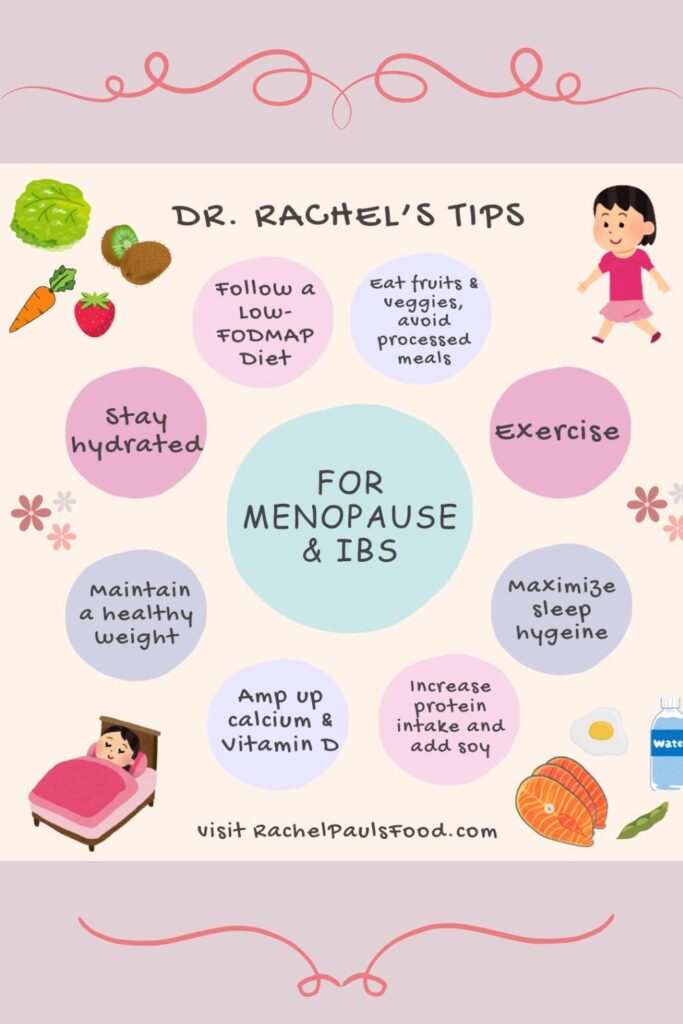
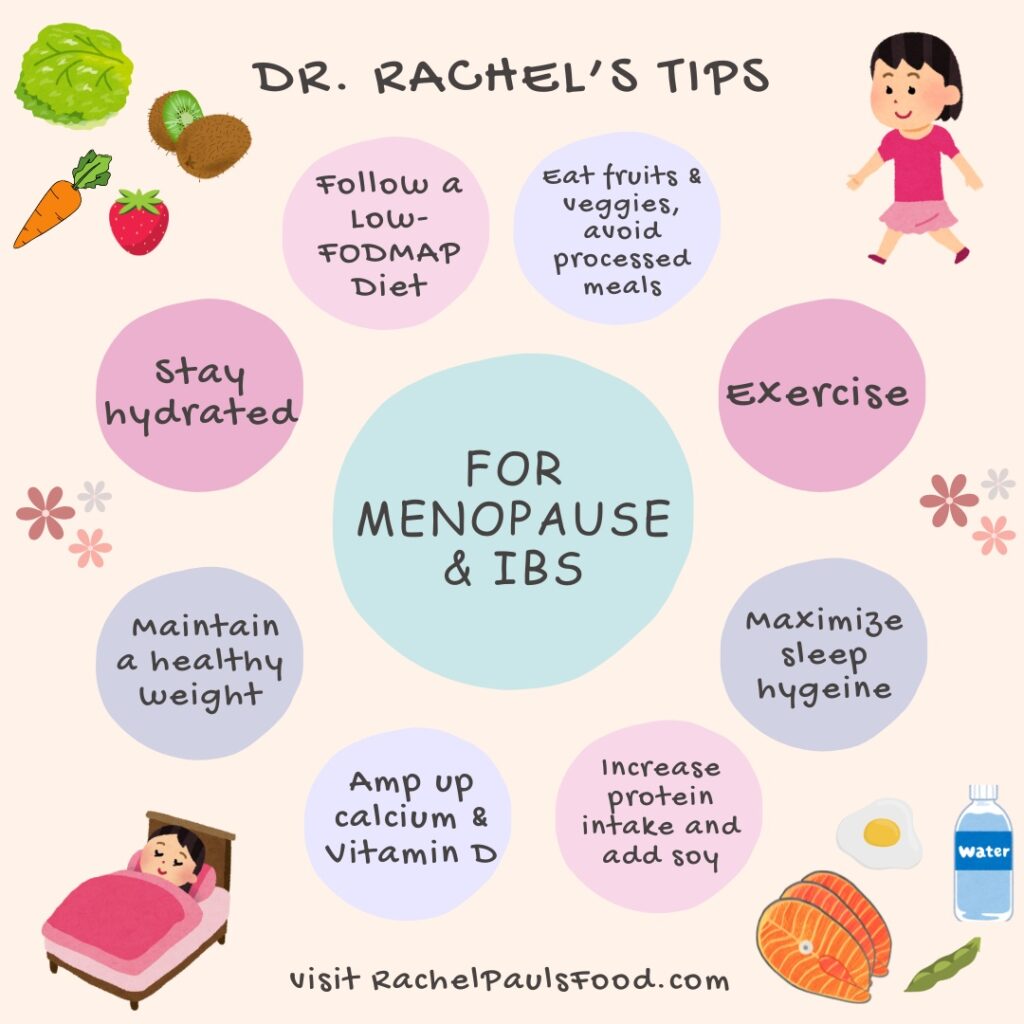
Dr Rachel’s Top 10 Tips to Improve Menopause Symptoms and Help Reduce IBS Flares
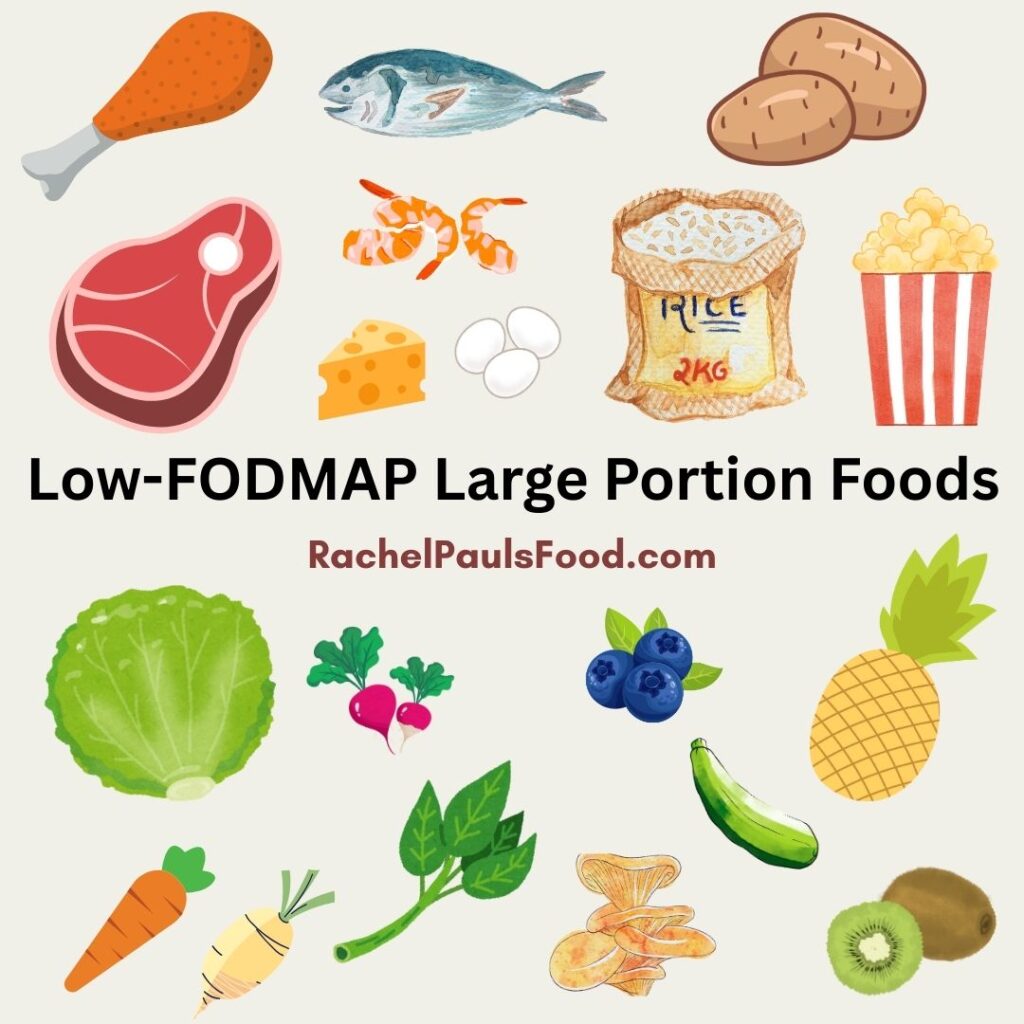
1. Avoid trigger foods and follow a low-FODMAP diet
-
- We all know how much diet can impact our IBS!!
- This may be a time for you to revert to a stricter ‘Elimination diet’ or cut back on some of the foods more likely to trigger symptoms FOR YOU (in my case, this may be avoiding the ‘cheat’ tastes of my kids desserts)
- If you aren’t on a low-FODMAP diet, this is a good time to try it! Check out my low-FODMAP Happy Gut Guide, low-FODMAP 5-Day Meal Plan or my low-FODMAP IBS Solution Cookbook to help you in your journey.
- Other gut irritants to reduce include: coffee, carbonated beverages (including sparkling water), alcohol, spicy foods, acidic foods, and cigarette smoking.
2. Get enough sleep
-
- Sleep is critical to feeling happy, energized and reducing stress. Not getting enough sleep leads to a diminished immune system and increase likelihood of IBS flares.
- Some ways to work on your sleep hygiene include:
- Going to bed and waking up at the same time each day
- Keeping your room dark at night (turn off the TV and leave your cell phone outside!)
- Exercising during the day
- Avoid large meals before bedtime
- Setting up a comfortable sleep environment (pillows, room temperature)
- During menopause, night sweats can make sleep even more challenging! I suggest making your room temperature and blankets as cool as possible. There are also special sweat-wicking pajamas and sheets, created for women with symptoms, that you may find helpful.
3. Maintain a healthy weight
-
- Weight gain is common during menopause. Alongside hormonal changes, aging changes can lower your metabolism. Unfortunately this means you have to move MORE and eat LESS to keep your normal shape. UGH!
- If you need to lose a few pounds, maybe this will be an incentive: losing weight has been shown to reduce hot flashes and night sweats!
- Many individuals find that increasing weight in the abdominal area (belly fat), can trigger IBS symptoms as well. See some of my tips to follow, to keep your weight stable during this key time.

4. Exercise!
-
- Regular exercise is essential. It helps control weight, improve energy and metabolism, reduce osteoporosis, maintain healthier joints and bones, decrease stress and improve sleep.
- This is a real winner!
- Even just 20 minutes, 3 times a week, can make a difference. Go for a walk, take a swim, play a round of tennis, or sweat through a yoga class. You will be glad you did!
5. Drink water
-
- Keeping hydrated is key to good bowel function, and can help maintain your weight. Plus, many women just don’t drink enough! I suggest about 8 glasses of water per day. Try to avoid coffee, which can be a gut irritant.
6. Eat plenty of fruits and vegetables
-
- As long as they are low-FODMAP (see my low-FODMAP Food List here), fruits and vegetables will help fill you up, and provide good balance for your gut microbiome. In turn, this will improve your overall health and reduce other symptoms of inflammation in your body.
- Check out my low-FODMAP Vegetable Stir Fry and low-FODMAP Smoothie recipes!
- As long as they are low-FODMAP (see my low-FODMAP Food List here), fruits and vegetables will help fill you up, and provide good balance for your gut microbiome. In turn, this will improve your overall health and reduce other symptoms of inflammation in your body.
7. Avoid processed foods
-
- NO-BRAINER! I think that the main reason why a low-FODMAP diet is SO beneficial, is that it naturally limits processed foods. There are so many things in packaged foods that can irritate your body and increase gut inflammation. Try to eat whole, natural foods, cook more at home, and limit mysterious ingredients (see my low-FODMAP Label Reading Guide for some tips)

8. Maximize protein intake
-
- Aging is associated with muscle loss, so amping up your protein (provided you stay within a healthy calorie intake), is beneficial to maintain a good body mass. Protein also helps maintain a full feeling to control weight.
- This is a delicious healthy low-FODMAP Zesty Grilled Chicken with Lime Recipe!
- Aging is associated with muscle loss, so amping up your protein (provided you stay within a healthy calorie intake), is beneficial to maintain a good body mass. Protein also helps maintain a full feeling to control weight.
9. Make sure to consume enough calcium and vitamin D
-
- Hormonal changes during menopause can cause bones to weaken, increasing the risk of osteoporosis, which no one wants!
- A diet rich in calcium and vitamin D is important to help prevent this bone loss:
- Even if you avoid lactose, it is possible to get these nutrients from milk alternatives, calcium enriched cereals, dark leafy greens (kale and spinach) or supplements if necessary (I love Adora Dark Chocolate Calcium discs).
10. Amp up your phytoestrogen intake
-
- Phytoestrogens are naturally occurring plant compounds that have estrogen-like effects in the body. Some low-FODMAP sources include soy (tofu, tempeh, edamame), flaxseeds, and sesame seeds.
- Many of these foods can be a healthy way to add a boost to your body’s natural balance. I do not recommend over-the-counter supplements containing phytoestrogens, unless directed by your physician.
- I have delicious low-FODMAP Pad Thai and low-FODMAP Vegetable Fried Rice with Tofu recipes!
Don’t forget to talk to your doctor about your symptoms, and share all the healthy changes you are making.
While not mentioned above, cutting back on smoking and alcohol is also recommended. I also suggest practice mindful techniques, and yoga for relaxation and stressful flares.
There is no way to avoid menopause, but with some lifestyle modifications, I hope I can navigate it successfully. Let me know how it works out for you!
- For some great low-FODMAP food ideas check out over 600 low-FODMAP Recipes on my blog. IBS-friendly!
Be healthy and happy,
Rachel Pauls, MD
References:
Margaret M. Heitkemper, PhD and Lin Chang, MD: Do Fluctuations in Ovarian Hormones Affect Gastrointestinal Symptoms in Women With Irritable Bowel Syndrome? Gend Med. 2009; 6(Suppl 2): 152–167.
Lenhart A, Naliboff B, Shih W, Gupta A, Tillisch K, Liu C, Mayer EA, Chang L.Postmenopausal women with irritable bowel syndrome (IBS) have more severe symptoms than premenopausal women with IBS.Neurogastroenterol Motil. 2020 May 29:e13913. doi: 10.1111/nmo.13913.
Heitkemper MM, Chang L.Do fluctuations in ovarian hormones affect gastrointestinal symptoms in women with irritable bowel syndrome? Gend Med. 2009;6 Suppl 2(Suppl 2):152-67.